Arthroscopy of the Knee Joint
INTRODUCTION
The knee is essentially made up of four bones. The femur or thighbone is the bone connecting the hip to the knee. The tibia or shinbone connects the knee to the ankle. The patella (kneecap) is the small bone in front of the knee and rides on the knee joint as the knee bends. The fibula is a shorter and thinner bone running parallel to the tibia on its outside. The joint acts like a hinge but with some rotation.
The knee is a synovial joint, which means it is lined by synovium. The synovium produces fluid lubricating and nourishing the inside of the joint.
Articular cartilage is the smooth surfaces at the end of the femur and tibia. It is the damage to this surface which causes arthritis.

Bones of the Knee Joint
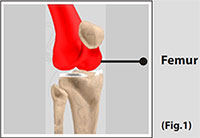
Femur
Femur The femur (thighbone) is the largest and the strongest bone in the body. It is the weight-bearing bone of the thigh. It provides attachment to most of the muscles of the knee.
(Refer fig. 1)
Condyle
The two femoral condyles make up for the rounded end of femur. Its smooth articular surface allows the femur to move easily over the tibial (shinbone) meniscus.
(Refer fig. 2)

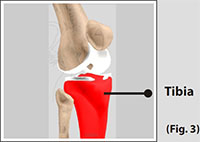
Tibia
The tibia (shinbone) the second largest bone in the body is the weight bearing bone of the leg. The menisci incompletely cover the superior surface of the tibia where it articulates with the femur. The menisci act as shock absorbers, protecting the articular surface of the tibia as well as assisting in rotation of the knee.
(Refer fig. 3)
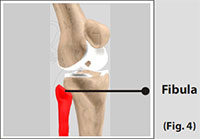
Fibula
The fibula, although not a weight bearing bone, provides attachment sites for the Lateral Collateral Ligaments (LCL) and the biceps femoris tendon. The articulation of tibia and fibula, also allows a slight degree of movement, providing an element of flexibility in response to the actions of muscles attaching to the fibula.
(Refer fig. 4)
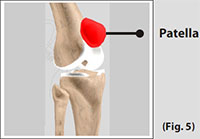
Patella
The Patella (kneecap), attached to the quadriceps tendon above and the patellar ligament below, rests against the anterior articular surface of the lower end of the femur and protects the knee joint.
The patella acts as a fulcrum for the quadriceps by holding the quadriceps tendon off the lower end of the femur.
(Refer fig. 5)
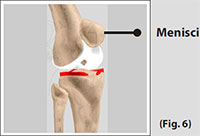
Menisci
The medial and the lateral meniscus are thin C-shaped layers of fibrocartilage, incompletely covering the surface of the tibia where it articulates with the femur. The majority of the meniscus has no blood supply and for that reason, when damaged the meniscus is unable to undergo the normal healing process that occurs in the rest of the body.
In addition, meniscus begins to deteriorate with age, often developing degenerative tears. Typically, when the meniscus is damaged, the torn pieces begin to move in an abnormal fashion inside the joint.
The menisci act as shock absorbers, protecting the articular surface of the tibia as well as assisting in rotation of the knee. As secondary stabilizers, the intact menisci interact with the stabilizing function of the ligaments and are most effective when the surrounding ligaments are intact.
(Refer fig. 6)
Fibrous Tissue of the Knee Joint
Anterior Cruciate Ligament (ACL)
The anterior cruciate ligament (ACL) is the major stabilizing ligament of the knee. The ACL is located in the center of the knee joint and runs from the femur (thigh bone) to the tibia (shin bone), through the center of the knee. The ACL prevents the femur from sliding backwards on the tibia (or the tibia sliding forwards on the femur). Together with Posterior Cruciate Ligament (PCL). ACL stabilizes the knee in a rotational fashion. Thus, if one of these ligaments is significantly damaged, the knee will be unstable when planting the foot of the injured extremity and pivoting, causing the knee to buckle and give way.
(Refer fig. 7)

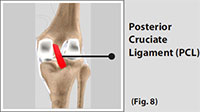
Posterior Cruciate Ligament (PCL)
Much less research has been done on the posterior cruciate ligament (PCL) because it is injured far less often than the ACL. The PCL prevents the femur from moving too far forward over the tibia. The PCL is the knee’s basic stabilizer and is almost twice as strong as the ACL. It provides a central axis about which the knee rotates.
(Refer fig. 8)
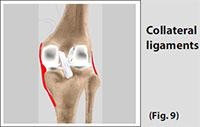
Collateral Ligaments
Collateral Ligaments prevent hyperextension, adduction, and abduction.
- Superficial MCL (Medial Collateral Ligament) connects the medial (inner) epicondyle of the femur to the medial condyle of the tibia and resists valgus (bending out) force.
- Deep MCL (Medial Collateral Ligament) connects the medial (inner) epicondyle of the femur with the medial meniscus.
- LCL (Lateral Collateral Ligament), entirely separate from the articular capsule, connects the lateral (outer) epicondyle of the femur to the head of the fibula and resists varus (bending in) force.
(Refer fig. 9)
Indications for Arthroscopy of the Knee Joint
Meniscal Cartilage Tears
Following a twisting type of injury the medial (or Lateral) meniscus can tear. This results either from a sporting injury or may occur from a simple twisting injury when getting out of a chair or standing from a squatting position. Our cartilages become a little brittle as we get older and therefore can tear a little easier.
The symptoms of a torn cartilage include
- Pain over the torn area i.e. inner or outer side of the knee
- Knee swelling
- Reduced motion
- Locking if the cartilage gets caught between the femur and tibia
Articular Cartilage(Surgery) Injury
If the surface cartilage is torn, this is most significant as a major shock-absorbing function is compromised. Large pieces of articular cartilage can float in the knee (sometimes with bone attached) and this causes locking of the joint and can cause further deterioration due to the loose body floating around the knee causing further wear and tear.
Most surface cartilage wear will ultimately lead to osteoarthritis. Mechanical symptoms of pain and swelling due to cartilage peeling off can be helped with arthroscopic surgery. The surgery smoothes the edges of the surface cartilage and removes loose bodies.
Cruciate Ligament Injuries
Rupture of the Anterior (rarely the posterior) Cruciate Ligament (ACL) is a common sporting injury. Once ruptured the ACL does not heal and usually causes knee instability and the inability to return to normal sporting activities. An ACL reconstruction is required and a new ligament is fashioned to replace the ruptured ligament. This procedure is performed using the arthroscope.
(Refer fig. 10)
Patella (knee-cap) disorders
Arthroscopy is sometimes useful in the treatment of patello-femoral problems of the knee. Looking directly at the articular cartilage surfaces of the patella and the patello-femoral groove is the most accurate way of determining how much wear and tear there is in these areas. Your physician can also watch as the patella moves through the groove, and may be able to decide whether or not the patella is tracking normally.
If there are areas of articular cartilage damage behind the patella that are creating a rough surface, special tools can be used by the surgeon to smooth the surface and reduce your pain. This procedure is sometimes referred to as shaving the patella.
The arthroscope can be used to treat problems relating to kneecap disorders, particularly mal-tracking and significant surface cartilage tears. Patients may need to stay overnight if a lateral release has been performed as knee swelling is quite common. The majority of common knee -cap problems can be treated with physiotherapy and rehabilitation.
(Refer fig. 10)

Inflammatory Arthritis
Occasionally arthroscopy is used in inflammatory conditions (e.g. Rheumatoid Arthritis) to help reduce the amount of inflamed synovium (joint lining) that is producing excess joint fluid. This procedure is called a synovectomy.
Bakers cysts
Bakers cysts or popliteal cysts are often found on clinical examination and ultrasound / MRI scans. The cyst is a fluid filled cavity behind the knee and in adults arises from a torn meniscus or worn articular cartilage in the knee. These cysts usually do not require removal as treating the cause (torn knee cartilage) will in most cases reduce the size of the cyst. Occasionally the cysts rupture and can cause calf pain. The cysts are not dangerous and do not require treatment if the knee is asymptomatic.
Autologous Chondrocyte Grafting
Isolated areas of articular cartilage loss can be repaired using cartilage transplant technology. This is a new and exciting field that is developing in the treatment of specific isolated cartilage defects in younger patients.
The process is called Autologous Chondrocyte Grafting. It involves harvesting cartilage cells from the affected knee, sending these cells to a laboratory and then culturing the cells to multiply into many cells. The large amount of cells produced are then placed back into the affected knee into the defect requiring resurfacing. Results are still short-term but are looking encouraging.
After a major cartilage or ligament injury has been treated the knee can return to normal function. There is however a small increase in the risk of developing long-term wear and tear (Osteoarthritis) and depending on the degree of injury activity modification may be required.
Activities that help prevent knees deteriorating quickly include:
- Low impact sports like swimming, cycling and walking
- Reducing weight and maintaining a healthy diet
What is Arthroscopy?
Arthroscopy is a surgical procedure in which an arthroscope is inserted into a joint. Arthroscopy is a term that comes from two Greek words, arthro-, meaning joint, and -skopein, meaning to examine.
Arthroscopy is performed in a hospital operating room under general anesthetic.
Surgical Procedure for Arthroscopy of the Knee Joint
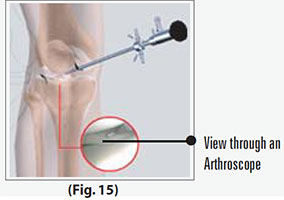
The arthroscope is a small fiber-optic viewing instrument made up of a tiny lens, light source and video camera. The surgical instruments used in arthroscopic surgery are very small (only 3 or 4 mm in diameter), but appear much larger when viewed through an arthroscope.
The television camera attached to the arthroscope displays the image of the joint on a television screen, allowing the surgeon to look, for example, throughout the knee-at cartilage and ligaments, and under the kneecap.
The surgeon can determine the amount or type of injury, and then repair or correct the problem, if it is necessary.
(Refer fig. 12)
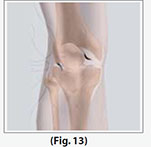
The surgeon makes two to three small incisions (about 1/4 of an inch), around the joint area. Each incision is called a portal. These incisions result in very small scars which in many cases are unnoticeable.
(Refer fig. 13)
In one portal, the arthroscope is inserted to view the knee joint. Along with the arthroscope, a sterile solution is pumped to the joint which expands the knee joint, giving the surgeon a clear view and room to work. The sterile solution is regulated by a drainage needle for the amount of fluid in the joint during the procedure.
(Refer fig. 14)
With the images from the arthroscope as a guide, the surgeon can look for any pathology or anomaly. The large image on the television screen allows the surgeon to see the joint directly and to determine the extent of the injuries and then to perform the particular surgical procedure if necessary.
(Refer fig. 15)
The other portal is used for the insertion of surgical instruments. A surgical instrument is used to probe various parts within the joint to determine the extent of the problem. If the surgeon sees an opportunity to treat a problem, a variety of surgical instruments can be inserted through this portal.
(Refer fig. 16)



After treating the problem, the portals (incisions) are closed by suturing or by tape. Arthroscopy is much less traumatic to the muscles, ligaments, and tissues than the traditional method of surgically opening the knee with long incisions (arthrotomy).
Post-operative recovery after Arthroscopy of the Knee Joint
- You will wake up in the recovery room and then be transferred back to the ward.
- A bandage will be around the operated knee.
- Once you are recovered your drip will be removed and you will be shown a number of exercises to do.
- Pain medication will be provided and should be taken as directed You can remove the bandage in 24 hours and place waterproof dressings (provided) over the wounds.
- It is NORMAL for the knee to swell after the surgery. Elevating the leg when you are seated and placing Ice-Packs on the knee will help to reduce swelling. (Ice packs on for 20 min 3-4 times a day until swelling has reduced)
- You are able to drive and return to work when comfortable unless otherwise instructed
- Please make an appointment 7-10 days after surgery to monitor your progress and remove piece on stitches.
Points of Interest
Why is arthroscopy necessary?
Diagnosing joint injuries and disease begins with a thorough medical history, physical examination, and usually X-rays. Additional tests such as an MRI, or CT scan may be needed. Through the arthroscope, a final diagnosis is made which may be more accurate than through “open” surgery or from X-ray studies.
What are the joints that can be viewed with an Arthroscope?
Although the inside of nearly all joints can be viewed with an arthroscope, six joints are most frequently examined with this instrument. These include the knee, shoulder, elbow, ankle, hip, and wrist. As engineers make advances in electronic technology and orthopaedic surgeons develop new techniques, other joints may be treated more frequently in the future.
What are the conditions that can be treated by arthroscopy?
Some problems associated with arthritis also can be treated. Several disorders are treated with a combination of arthroscopic and standard surgery.
Diseases and injuries can damage bones, cartilage, ligaments, muscles, and tendons. Some of the most frequent conditions found during arthroscopic examinations of joints are:
- Inflammation
- Synovitis – inflamed lining (synovium) in knee, shoulder, elbow, wrist, or ankle.
- Injury
- Acute and chronic Shoulder – rotator cuff tendon tears, impingement syndrome, meniscal (cartilage) tears, chondromalacia (wearing or injury of cartilage cushion), and anterior cruciate ligament tears with instability Wrist – carpal tunnel syndrome
- Loose bodies of bone and/or cartilage – knee, shoulder, elbow, ankle, or wrist.
What are the Possible Risks & Complications of Arthroscopy of the Knee Joint?
- General anesthetic risks are extremely rare. Occasionally patients have some discomfort in the throat as a result of the tube that supplies oxygen and other gasses. Please discuss with the anesthetist if you have any specific concerns.
Risks related to Arthroscopic knee surgery include:
- Post-operative bleeding
- Deep Vein Thrombosis (DVT)
- Infection
- Stiffness
- Numbness to part of the skin near the incisions
- Injury to vessels, nerves and a chronic pain syndrome
Progression of the disease process
The risks and complications of arthroscopic knee surgery are extremely small. One must however bear in mind that occasionally there is more damage in the knee than was initially thought and that may affect the recovery time. In addition if the cartilage in the knee is partly worn out then arthroscopic surgery has about a 65% chance of improving symptoms in the short to medium term but more definitive surgery may be required in the future. In general arthroscopic surgery does not improve knees that have well established Osteoarthritis.
What are the Advantages of Arthroscopy of the Knee Joint?
Although arthroscopic surgery has received a lot of public attention because it is used to treat well-known athletes, it is an extremely valuable tool for all orthopaedic patients and is generally easier on the patient than “open” surgery. Most patients have their arthroscopic surgery as outpatients and are home several hours after the surgery.
Recovery after Arthroscopy of the Knee Joint
The operative dressing can usually be removed 48hs after surgery but has to be kept clean and dry. Leave adhesive over incisions alone.
Although the puncture wounds are small and pain in the joint that underwent arthroscopy is minimal, it takes several weeks for the joint to maximally recover. A specific activity and rehabilitation program may be suggested to speed your recover and protect future joint function.
It is not unusual for patients to go back to work or school or resume daily activities within a few days. Athletes and others who are in good physical condition may in some cases return to athletic activities within a few weeks.
Remember, though, that people who have arthroscopy can have many different diagnoses and preexisting conditions, so each patient’s arthroscopic surgery is unique to that person. Recovery time will reflect that individuality.
